Connect With Us
Super User
Different Levels of Foot Wounds
 An open sore on the foot is known as a foot ulcer. It can be common among diabetic patients who have cuts on their feet, which they may not be aware of. A simple cut may develop into a foot ulcer as a result of neuropathy, which causes the inability to feel existing wounds, cuts, or scrapes on the feet. There are varying degrees of foot ulcers, which can range from a shallow wound that is on the surface to a deep wound involving the tendons and bones. Any type of wound on the foot needs prompt medical attention, and this may prevent a foot ulcer from developing. A wound on the foot is treated by cleaning out debris that may be inside of it. This is followed by tightly wrapping it with a bandage that can protect the foot, and it is beneficial to elevate it as often as possible. The more shallow the wound is, the greater the chances of a complete healing is possible. If you have a foot wound, please consult with a podiatrist who can offer the correct treatment methods for wound care.
An open sore on the foot is known as a foot ulcer. It can be common among diabetic patients who have cuts on their feet, which they may not be aware of. A simple cut may develop into a foot ulcer as a result of neuropathy, which causes the inability to feel existing wounds, cuts, or scrapes on the feet. There are varying degrees of foot ulcers, which can range from a shallow wound that is on the surface to a deep wound involving the tendons and bones. Any type of wound on the foot needs prompt medical attention, and this may prevent a foot ulcer from developing. A wound on the foot is treated by cleaning out debris that may be inside of it. This is followed by tightly wrapping it with a bandage that can protect the foot, and it is beneficial to elevate it as often as possible. The more shallow the wound is, the greater the chances of a complete healing is possible. If you have a foot wound, please consult with a podiatrist who can offer the correct treatment methods for wound care.
Wound care is an important part of dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with one of our clinicians from The Footcare Centre. Our podiatrists will assess your condition and provide you with quality treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the utmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover it with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions please feel free to contact our offices located in Weybridge, UK. We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a podiatrist—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
What Does Sesamoiditis Feel Like?
 Sesamoiditis is a foot condition that you might have heard of. It can occur in an individual when the two small sesamoid bones in the ball of the foot become inflamed. Interestingly, these two bones do not directly connect to any other bones. Rather, the sesamoid bones connect to tendons and muscles. When an individual has sesamoiditis, they may feel any number of symptoms. Most commonly, a patient might feel some kind of pain in the forefoot. This pain may be especially pronounced when putting weight on the feet. Additionally, a patient with sesamoiditis may unintentionally shift the weight of their body to the outside of their feet to avoid putting weight on the sesamoids when walking. These are just some of the many different symptoms that patients with sesamoiditis might demonstrate. Contact your podiatrist today for more information.
Sesamoiditis is a foot condition that you might have heard of. It can occur in an individual when the two small sesamoid bones in the ball of the foot become inflamed. Interestingly, these two bones do not directly connect to any other bones. Rather, the sesamoid bones connect to tendons and muscles. When an individual has sesamoiditis, they may feel any number of symptoms. Most commonly, a patient might feel some kind of pain in the forefoot. This pain may be especially pronounced when putting weight on the feet. Additionally, a patient with sesamoiditis may unintentionally shift the weight of their body to the outside of their feet to avoid putting weight on the sesamoids when walking. These are just some of the many different symptoms that patients with sesamoiditis might demonstrate. Contact your podiatrist today for more information.
Sesamoiditis is an unpleasant foot condition characterized by pain in the balls of the feet. If you think you’re struggling with sesamoiditis, contact one of our clinicians from The Footcare Centre. Our podiatrists will treat your condition thoroughly and effectively.
Sesamoiditis
Sesamoiditis is a condition of the foot that affects the ball of the foot. It is more common in younger people than it is in older people. It can also occur with people who have begun a new exercise program, since their bodies are adjusting to the new physical regimen. Pain may also be caused by the inflammation of tendons surrounding the bones. It is important to seek treatment in its early stages because if you ignore the pain, this condition can lead to more serious problems such as severe irritation and bone fractures.
Causes of Sesamoiditis
- A sudden increase in activity
- Increase in a physically strenuous movement without a proper warm-up or build-up
- Foot structure: those who have smaller, bonier feet or those with a high arch may be more susceptible
Treatment for sesamoiditis is non-invasive and simple. Podiatrists may recommend a strict rest period where the patient forgoes most physical activity. This will help give the patient time to heal their feet through limited activity. For serious cases, it is best to speak with your podiatrist to determine a treatment option that will help your specific needs.
If you have any questions please feel free to contact our offices located in Weybridge, UK. We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Sesamoiditis
Sesamoiditis is a condition in which the sesamoid bones in the forefoot become inflamed from physical activity. Sesamoid bones are bones that are not connected to other bones but are located in tendons or muscles. Two of these sesamoid bones are very small and located on the underside of the foot near the big toe. Athletes such as runners, baseball and football players, and dancers are likely to experience sesamoiditis. Those with high-arched feet, flat feet, or runners who run on the ball of their feet are also prone to suffer from sesamoiditis.
Symptoms include pain or throbbing on the ball of the foot near the big toe. The pain generally starts with a mild throbbing but gradually builds up to shooting pain. Bruising, swelling, and redness are possible, but in most cases, these symptoms are not present. However, moving the big toe can result in pain and difficulty.
To conduct a diagnosis, the podiatrist will examine the ball of the foot and big toe. They will look for any outliers and check the movement of the toe. X-rays will be taken to rule out any other conditions and ensure that it is sesamoiditis.
Treatment for sesamoiditis is generally mild and includes rest, anti-inflammatory and pain medication, and ice treatments to deal with the swelling and pain. Orthotics may be needed with people who have flat or high-arched feet to relieve pressure off the bones. In some cases, the toe will be taped and immobilized to allow healing. The podiatrist may also decide to use a steroid injection to help with swelling as well. If you have sesamoiditis, you shouldn’t engage in any intensive activity, as it may inflame the area and worsen your pain. If the sesamoid bone has fractured, surgery may be required to remove the sesamoid bone.
If you are suffering from sesamoiditis or are experiencing symptoms similar to sesamoiditis, you should stop all physical activity that puts strain on the area. Furthermore, you should see a podiatrist for a diagnosis to see if you have sesamoiditis.
Two Types of Toe Fractures
 There are different ways of fracturing a toe. A sudden increase in running or walking can produce a stress or hairline fracture, and can be uncomfortable. When a heavy object is dropped on it, or if it is jammed against a piece of furniture, it is considered to be more of a serious fracture, and there are noticeable symptoms that a break has occurred. These can include immediate bruising, and swelling, and the affected toe bone may protrude from the skin. If the break is very painful, a popping sound may be heard at the time of the injury. There is often a limited range of motion, and it can be difficult to walk. A proper diagnosis often consists of having an X-ray taken, and this is generally successful in determining how severe the break is. Many broken toes are treated by using the buddy taping method. This involves taping the broken toe to the toe next to it, which can provide the stability that is needed as the healing process occurs. If you have broken your toe, it is strongly suggested that you schedule an appointment with a podiatrist as quickly as possible, so the toe can heal correctly.
There are different ways of fracturing a toe. A sudden increase in running or walking can produce a stress or hairline fracture, and can be uncomfortable. When a heavy object is dropped on it, or if it is jammed against a piece of furniture, it is considered to be more of a serious fracture, and there are noticeable symptoms that a break has occurred. These can include immediate bruising, and swelling, and the affected toe bone may protrude from the skin. If the break is very painful, a popping sound may be heard at the time of the injury. There is often a limited range of motion, and it can be difficult to walk. A proper diagnosis often consists of having an X-ray taken, and this is generally successful in determining how severe the break is. Many broken toes are treated by using the buddy taping method. This involves taping the broken toe to the toe next to it, which can provide the stability that is needed as the healing process occurs. If you have broken your toe, it is strongly suggested that you schedule an appointment with a podiatrist as quickly as possible, so the toe can heal correctly.
Broken toes may cause a lot of pain and should be treated as soon as possible. If you have any concerns about your feet, contact one of our clinicians from The Footcare Centre. Our podiatrists will assess your condition and provide you with quality treatment.
What Is a Broken Toe?
A broken toe occurs when one or more of the toe bones of the foot are broken after an injury. Injuries such as stubbing your toe or dropping a heavy object on it may cause a toe fracture.
Symptoms of a Broken Toe
- Swelling
- Pain (with/without wearing shoes)
- Stiffness
- Nail Injury
Although the injured toe should be monitored daily, it is especially important to have a podiatrist look at your toe if you have severe symptoms. Some of these symptoms include worsening or new pain that is not relieved with medication, sores, redness, or open wounds near the toe.
If you have any questions please feel free to contact our offices located in Weybridge, UK. We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What to Know About a Broken Toe
The forefoot is composed of five metatarsal bones and fourteen phalanges. Each toe has three phalanges except for the big toe which only has two. Our toes play an essential role in the walking process, which is why a broken toe could seriously disrupt one’s ability to move around. Toe fractures are common and can be very painful. Fortunately, these injuries rarely require surgery and usually heal with rest and a change in activity.
Broken toes typically result from a traumatic event such as falling, stubbing the toe, or dropping something on the toe. Traumatic toe fractures may be categorized as either minor or severe fractures. At times, one may hear a “pop” or “crack” sound when the bone breaks. Common symptoms of a traumatic toe fracture include pain, throbbing, bruising, swelling, and redness.
Another type of toe fracture is a stress fracture. These injuries usually appear in the form of small hairline breaks on the bone. Stress fractures develop after repetitive activity instead of a single injury. Stress fractures occur when the muscles in the bone become too weak to absorb impact. Consequently, the toe bone becomes vulnerable to any pressure and impact it endures. Symptoms of a stress fracture in the toe include swelling without bruising, tenderness to the touch, pain that goes away with rest, and pain after walking or running.
If you suspect that you have a broken toe, you should make an appointment with your podiatrist. He or she will likely diagnose you by performing a physical exam and an X-ray. Treatment for a broken toe may include the R.I.C.E. method, buddy taping, surgery, or antibiotics. The R.I.C.E. method (Rest, Ice, Compression, and Elevation) is a common treatment method for many injuries because it decreases pain. Buddy tapping involves wrapping the injured toe next to an adjacent toe to keep it supported and protected. These two methods have proven to be effective in the healing process for toe fractures. The estimated healing time for a broken toe is approximately four to six weeks. If the injury becomes infected or requires surgery, the estimated healing time may take eight weeks or more.
Plantar Fasciitis and Swimming
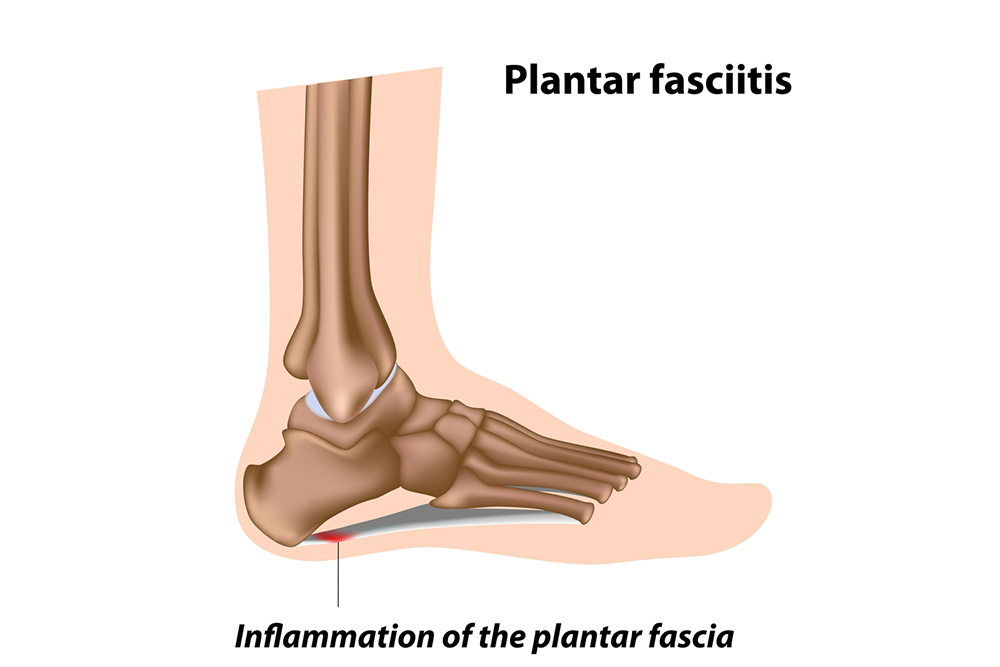 One of the most common forms of heel pain that a podiatrist will encounter in patients is known as plantar fasciitis, a condition where the plantar fascia becomes inflamed. Many physical activities and sports may exacerbate this condition, particularly if it is high impact. However, in some respects, swimming may seem to be a helpful alternative for those with plantar fasciitis. Swimming is particularly low impact, enabling the athlete to burn calories while often not placing high pressure on the feet. It is important to note, however, that if someone has plantar fasciitis, it is possible that they still may experience pain when engaging in this activity. Someone with a particularly bad case of plantar fasciitis may feel pain if they try to push off of the wall with their feet when swimming. Schedule an appointment today with a podiatrist to learn more about plantar fasciitis.
One of the most common forms of heel pain that a podiatrist will encounter in patients is known as plantar fasciitis, a condition where the plantar fascia becomes inflamed. Many physical activities and sports may exacerbate this condition, particularly if it is high impact. However, in some respects, swimming may seem to be a helpful alternative for those with plantar fasciitis. Swimming is particularly low impact, enabling the athlete to burn calories while often not placing high pressure on the feet. It is important to note, however, that if someone has plantar fasciitis, it is possible that they still may experience pain when engaging in this activity. Someone with a particularly bad case of plantar fasciitis may feel pain if they try to push off of the wall with their feet when swimming. Schedule an appointment today with a podiatrist to learn more about plantar fasciitis.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our clinicians from The Footcare Centre. Our podiatrists can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your podiatrist right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our offices located in Weybridge, UK. We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Read More About Plantar Fasciitis
Plantar Fasciitis
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk of developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
Best Shoes for People With Heel Spurs
 Heel spurs are small, bony growths caused by excessive calcium deposits forming on the heel of the foot. These can grow on the bottom of the heel or the heel bone where the plantar fascia ligament attaches the heel to the toes. This connective tissue keeps the foot in a comfortable arch position, but a heel spur can damage the fibrous tissue and it will not be able to perform its job. In addition to causing every step one takes to be painful, heel spurs can cause long-term foot problems. Trying to purchase shoes that accommodate heel spurs can be an overwhelming task, yet it is imperative to wear proper footwear. When choosing footwear to alleviate pain and prevent further damage from heel spurs, it is crucial to look for shoes with firm rearfoots or backs of shoes. These are less apt to bend during movement and thus provide more support to the heel. Shoes should also have additional cushioning and a flexible forefoot that bends and stretches easily with movement. If you suffer from heel spurs, consult with a podiatrist who can help you with treating this condition, as well as suggest the best footwear to help with pain and prevention.
Heel spurs are small, bony growths caused by excessive calcium deposits forming on the heel of the foot. These can grow on the bottom of the heel or the heel bone where the plantar fascia ligament attaches the heel to the toes. This connective tissue keeps the foot in a comfortable arch position, but a heel spur can damage the fibrous tissue and it will not be able to perform its job. In addition to causing every step one takes to be painful, heel spurs can cause long-term foot problems. Trying to purchase shoes that accommodate heel spurs can be an overwhelming task, yet it is imperative to wear proper footwear. When choosing footwear to alleviate pain and prevent further damage from heel spurs, it is crucial to look for shoes with firm rearfoots or backs of shoes. These are less apt to bend during movement and thus provide more support to the heel. Shoes should also have additional cushioning and a flexible forefoot that bends and stretches easily with movement. If you suffer from heel spurs, consult with a podiatrist who can help you with treating this condition, as well as suggest the best footwear to help with pain and prevention.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact one of our clinicians from The Footcare Centre. Our podiatrists will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching to the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main conditions spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of the weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions please feel free to contact our offices located in Weybridge, UK. We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.